New Israeli technology improves prediction of patient response to immunotherapy
Ben-Gurion University researchers develop innovative biosensor, team up with Israeli biotech company OncoHost in bid for FDA approval
Renee Ghert-Zand is a reporter and feature writer for The Times of Israel.
Researchers at Ben-Gurion University of the Negev have developed a new bio-sensing technology that predicts cancer patients’ response to immune checkpoint inhibitor (ICI) immunotherapy. More accurate and easier to implement than current methods, the technology has the potential to improve the effectiveness of immunotherapy and spare patients toxicity and debilitating side effects.
The bioassay was developed by a team led by Prof. Moshe Elkabets and Prof. Angel Porgador from the Faculty of Health Sciences at BGU, along with collaborators from Soroka Medical Center in Beersheva and Barzilai Medical Center in Ashkelon. The results of their study were recently published in the peer-reviewed Science Advances journal.
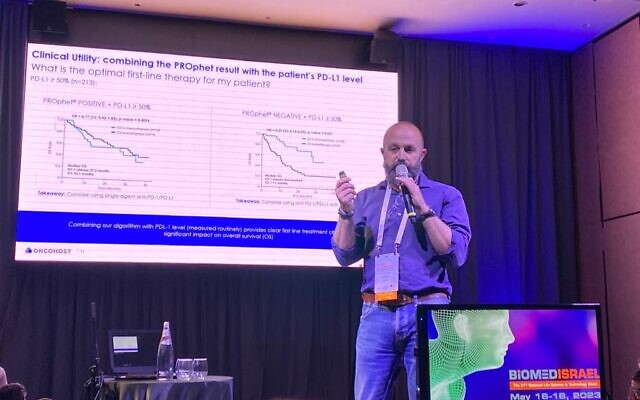
The new Immuno-checkpoint Artificial Reporter (IcAR) technology has been licensed to OncoHost, an Israeli-guided oncology company, which will seek US Food and Drug Administration approval. OncoHost CEO Dr. Ofer Sharon told The Times of Israel he expects clinical trials to begin in six to eight months and hopes the product will reach the market in no more than two years.
“This product has a huge potential. It is very exciting and we have an ambitious plan for it,” Sharon said.
Immunotherapy is a treatment that boosts the body’s immune system to help find and destroy cancer cells. Depending on a patient’s case, it can be combined with other treatments such as chemotherapy, radiotherapy, and surgery. The research and medical communities are enthusiastic about the potential for immunotherapy and hundreds of drug trials are ongoing in the US. However, immunotherapy is currently approved for only some 20 kinds of cancer. Also, the response rate is only 20-40 percent and the treatment can lead to toxicity and side effects that negatively impact quality of life.
ICI is one of several kinds of immunotherapy. It involves introducing monoclonal antibody drugs via infusion into a vein. These drugs are designed to break down the protein “checkpoints” that cancer cells create to protect themselves from antibodies that seek to destroy them.

The most common ICI is called anti-PD1. The therapy interferes with the tumor’s attempts to suppress the immune system’s T cells’ ability to attack the cancer. T cells have a PD1 protein “off switch” that tells the T cells to leave the other cells alone. This switching off happens when the PD1 receptor binds to the other cells’ PDL1 or PDL2 ligands (also proteins).
Cancer cells tend to have many PDL1 and PDL2 ligands, so they can evade attack from the T cells. This is the “checkpoint” that the cancer cells put up to defend themselves. The anti-PD1 agent given in ICI therapy prevents the binding of the ligands and receptors and boosts the body’s immune response.
“The therapy prevents the ability of the tumor to escape the anti-tumor immunity,” explained Elkabets.
Before now there existed biomarkers to predict the success of ICI on a patient, but these tests had only a 10-15% response, according to Elkabets.
“The difference with our bioassay is that it looks for functionality. The other technologies looked only for the expression of proteins,” Elkabets said.
“Maybe expression matters. But what’s more important is the functionality of the binding of the ligands and receptors. You need to know how many of the ligands can suppress the T cells. You can have a lot of proteins and not many are active, and have few but many of those are very active,” he said.
OncoHost’s Sharon explained that the researchers developed an artificial body based on a T cell (the IcAR) and expressed PD1 on its surface. They incubated this cell with a tumor and looked to see if the cell was secreting an easily measured specific substance, Interleukin-2 (IL-2). The secretion happens only when the PD1 is active.
“So what we have now is an assay that allows us to identify functionality based on the secretion of the increase in the levels of IL-2. It’s basically a new biosensor,” he said.
The BGU team was able to quantify the functionality of the protein in a fixed tissue, or old pathology sample. This is a clear advantage over current technologies that involve screening fresh tissue samples, meaning that patients have to undergo several biopsies over time.
“With our technology, I can take samples from pathologies from 10 years and I can do retrospective studies of thousands and thousands of patients to look for new potential patients that can respond to treatment. This will help us select the right patients with different cancer types. There is an unlimited opportunity with this technology,” Elkabets said.

Both Elkabets and Sharon emphasized that this new technology is not only for PD1 and can be adapted to other proteins found on T cells, including CTLA-4 and others.
“I think that we will be able to potentially use this technology to identify immune checkpoint combination therapies,” Elkabets said.
As he prepares to engage with the FDA, Sharon is pleased with the data on hand.
“What we have is something with very high sensitivity specificity as compared to the current PDL1 biomarker… and we have the results already from several tumor types — lung, metabolic, renal cell, and melanoma — with similar performance,” Sharon said.
“So different tumor types, better accuracy, and a tool that I think is scalable at relatively low cost,” he said.










